Sitaram Bhartia Institute of Science & Research
B-16, Qutab Institutional Area, New Delhi, 110016
+91-9811109833, 9810446857
Shoulder Dislocation (Video Link - Shoulder Dislocation)
Know your shoulder

Shoulder joint is a ball-and-socket joint (Fig 1). The socket is small and shallow (called glenoid), and the ball, formed by upper end of arm bone (humerus), is round and big. This design feature (big ball and small socket) makes the shoulder a versatile mobile joint making it possible to take the hand in a nearly 360 degree plane (Fig-2). The down side of this design is that it makes the joint inherently unstable. Therefore, shoulder is the most common joint to dislocates. Nearly 1 in 1000 persons dislocate their shoulder at sometime in life.

The stability of shoulder joint is determined by the connecting ligaments and muscles. Ligaments are thickened, ribbon-like part of the tissues enveloping the shoulder (Fig 3). These get tightened when the shoulder is taken to extreme positions, and hence prevent dislocation. The other stabilisers of the shoulder are the muscles surrounding the shoulder.
These muscles, by synchronised contractions keep the shoulder in place. Any deficiency in tissues connecting the ball to the socket or dysfunctional muscle contractions make the shoulder wander away. This may present as a small problem of feeling the shoulder go in and out (subluxation), or in the extreme form, a full-fledged dislocation.
Why does the shoulder dislocate?
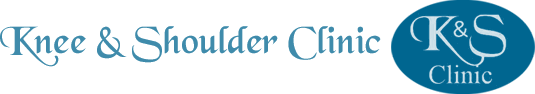
Most common reason for shoulder to dislocate is injury such as fall on an out-stretched hand. When this happens, there occurs detachment of the labrum from the socket (Fig 4a & b). Labrum is a rim of thick rubber-like tissue all around the edge of the glenoid. something akin to a rubber washer in a pressure cooker. This helps in gripping the head in the socket. This does not allow shoulder to come out of the socket and when it gets detached the shoulder comes out. Once the shoulder is put back (by doctors or by the patient himself), the labrum falls back in place and heals up in 50 percent patients, and in such cases, the shoulder never dislocates again. In cases where, the labrum does not fall back and does not heal, it becomes a weak point in the restraints of shoulder. Anytime the shoulder moves in a particular direction, it may come again through the weak area. This may happen again and again.
Frequency of repeated dislocation varies from patient to patient, and depends upon a lot of factors. The well understood factors are as follows:
a) Age of the patient – patient under 20 years tend to dislocate their shoulder repeatedly 80% of times. This tendency reduces with age.
b) Genetic constitution of the patient – some patients genetically have tissue laxity, and their shoulder dislocate rather easily on minor provocation.
c) Associated bony defect – sometimes, the capsule detaches from the glenoid along with a chip of bone from the glenoid. If this chip is of sufficient size, recurrent dislocation happens.
Can a repeatedly dislocating shoulder be cured by medicines or physiotherapy?
The chances of dislocation happening can be reduced by avoiding certain overhead activities such as sports demanding overhead action (Volleyball, Basketball etc). It can also be controlled to some extent by strengthening the muscles around the shoulder. There are no medicines which can heal the torn labrum, nor can physiotherapy heal it. In most young and active persons, it tends to recur anyway. One reason which increases the chances of that happening is also the damage to the bone part of the ball and the socket.
What does surgical treatment entail?
Surgery consists of attaching the torn labrum back to where it belongs. This has been done since ages by open surgery, whereby the torn labrum is re-attached to the glenoid rim by drilling holes in the glenoid and tying the labrum to the rim. In the current technique, the same is done by key-hole surgery (arthroscopic surgery). In this technique no open surgery is involved. The surgery is done under general anaesthesia. Three small cuts (1 cm in size) are made on the shoulder. Through these, three cannulas are introduced. Through one these is introduced a small camera, and through others, micro instruments are introduced.

The benefit of key-hole surgery are: less pain, less cutting, quicker recovery, and fewer complications (Fig-6). Anchors are used to tie ligaments to the bone. Anchors are devices which are drilled into the bone. These carry sutures on their head. Bite is taken through the torn tissue with special tools and thus sutures are passed through the torn tissue. By special knotting techniques, the torn tissues are tied to the labrum. All this is done through key-holes without opening the joint. In vast majority it is possible to repair the tissues by this technique, but occasionally, opening may be required for better repair.
How much time does the operation take?
Actual operation takes about 1 hour, but pre-op preparation (anaesthesia, positioning etc.) takes another one hour. AGer surgery, you are kept in recovery area, and shifted to the room once you are fully awake. Post operation you will be in a sling for a few weeks.
Is it a painful operation?
The operation is done under general anaesthesia, hence no pain at all while operating. In the post op period we control the pain by intra venous pain relieving medicines. On a scale of 0-10, we are able to keep the pain within less than 3 range, which is very much tolerable.
How much does it cost?
Cost varies from case to case, depending upon the size of the tear. On an average, it costs from 1.5 L to 2.0 Lac*. Exact estimate can be taken for your particular case. We will be able to give you an estimate at the time of finalising the date.
How successful is the operation?
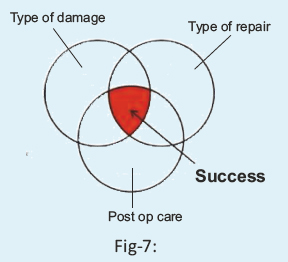
It is overall a successful operation. Our data shows that 97% do good aGer 5 years of surgery. The success depends upon the following factors (Fig-7):
- The type of damage
- The type of repair
- Post op care
Any of the three not working well can lead to failure. Failure may mean partial success or no success. Fortunately, good over 97% heal up well, and are able to do all the activities after 6 months.
How much time does it take to recover?
In a usual case, immobilisation in a simple sling is done for 2 weeks. One can take the arm out of sling daily for bathing. It is preferable to wear easy to wear front open clothes. Eating and typing is possible from day 2 but the shoulder cannot be liGed for 2 weeks. One can perform day-to-day functions after 2 weeks. Post-op home-based physiotherapy is required for a period of 4 weeks. Eventually patients get full range of motion (Fig-8). Sports are prohibited for 6 months.
What are the possible risks of surgery?
The surgery is generally safe. There are some standard risks which are associated with any surgery. Some of these are mentioned below for the sake of completion, and not to alarm.

Anaesthesia Risk: There are risks of putting anybody under anaesthesia. These range from as minor as nausea and vomiting due to some medication, to serious complications such as drug reaction.
Surgical risk: The only serious risk is infection, which occurs in only 1 in 500 patients. We take all precautions to keep it within reasonable limits. The other risks are recurrence of dislocation (2/100) and stiff shoulder (2/100).
What are the highlights of our technique ?
- We use one-time use (disposable) tools to maintain lowest possible risk of infection.
- We use anchorless sutures, what are called all-suture anchor. There is nothing foreign inside the shoulder.
- We have extensive experience of having repaired extreme forms of dislocations (often even more than 25% bone loss), arthroscopically.
- Allow controlled movements of the shoulder, next day. This is because the repair we do is robust.
- Allow bath the very next day.
- We have devised a home-based physiotherapy programme with only a few visits to our shoulder trained physios.
- The surgeon and physio work in close coordination.
- The surgeon is available 24X7, in case of any emergency.
- We give a recording of the whole operation.
Our philosophy: Most important, we have a philosophy of treatment. We take every patient as a human being with different requirements – physical and psychological. We customize our treatment to patient's need. Our aim is to give our patient the experience of having gone through the treatment, what we would expect for our own relative. For us, by choosing us their doctor, the patient is giving us a great honour, and we value it. To showcase that we care, all our operated patients have direct access to cellphones of our team, including that of the chief surgeon.
Shown below are the shoulders of two patients, one operated by open surgery and the other by arthroscopic surgery.