Sitaram Bhartia Institute of Science & Research
B-16, Qutab Institutional Area, New Delhi, 110016
+91-9811109833, 9810446857
Rotator Cuff Tear (Video Link - Rotator Cuff Tear)
What is rotator cuff?

Shoulder joint is a ball and socket joint. The socket is small and hollow (called glenoid), and the ball is round and big (formed by upper end of the arm bone called humerus). This design feature (big ball and small socket) makes the shoulder a versatile joint, and this is the reason that it is possible to take the arm in nearly 360˝ plane.
The ball is held in the socket with the help of ligaments and muscles. There are two group of muscles controlling the shoulder - the deep group and the superficial group.  The deep group of muscles run from shoulder blade to the ball of the shoulder, and form a kind of hood (cuff) around the head. (Fig. 3) These are called rotator cuff MUSCLES. These are a group of four muscles - from front to back Subscapularis, Supraspinatus, Infraspinatus and Teres minor. The essential functions of these muscles is to keep the head centred in the glenoid so that the rest of the muscles can effectively move the shoulder. It is supraspinatus which is torn most frequently.
The deep group of muscles run from shoulder blade to the ball of the shoulder, and form a kind of hood (cuff) around the head. (Fig. 3) These are called rotator cuff MUSCLES. These are a group of four muscles - from front to back Subscapularis, Supraspinatus, Infraspinatus and Teres minor. The essential functions of these muscles is to keep the head centred in the glenoid so that the rest of the muscles can effectively move the shoulder. It is supraspinatus which is torn most frequently.
How does the rotator cuff get torn?

Rotator cuff gets torn due to unexpected pull of the muscles. This may happen due to fall on an out stretched hand, or due to some sudden jerk to the shoulder. Tears, where primary reason for tear is injury, are called traumatic tears (Fig.4). Sometimes, a muscle can tear even without an injury. This happens due to age-related weakness of tendons. Such tendons break for no reason, or even with minimal injury. These are called degenerative tears. Also, there are in-between tears where, in the background of degeneration, a minor injury leads to tear. The quality of tear and it's healing potential depends upon the type of tear.
How does one come to know that the cuff has torn?

Usually there is a history of injury followed by pain in the shoulder. One may notice that it's not possible to liG the shoulder. It's common that one considers it a 'minor sprain', and expects it to get better by itself. Not finding any improvement, oGen an x ray is done, which does not show anything abnormal (as x ray only show broken bones and not torn tendons). Falsely reassured by 'no fracture', most patients wait further or go for physiotherapy. In either case, improvement does not occur. It is at this stage that they either consult an orthopaedic surgeon, who suspects a cuff tear and gets an MRI done, or sometimes the patient himself walks into an MRI centre, and gets an MRI done. It is here, to their shock, they are told that they have tendon rupture (Fig. 5).
Often, the patient may complain of pain as the only symptom, without any known injury or fall. OGen such cases are diagnosed initially as 'Frozen shoulder', and patients are advised to go for physiotherapy. It's only when they don't improve in due course (and sometimes even deteriorate), that they get an MRI done, and what was thought to be a 'Frozen shoulder' comes out to be a cuff tear.
Can a torn cuff heal up by itself?
A minor, partial cuff tear may heal up with rest. Complete tear, more often than not, progresses in size. One can live with a small cuff tear by strengthening muscles around the shoulder and by avoiding forceful movements. This may be possible in elderly people and in those in sedentary life style, but is diffcult in more active people. In the later, more often than not, the tear progresses in size, the torn muscle gets weak (atrophied), and the difficulty increases with time. In fact, with undue wait, the possibility of repair and retraining of torn muscles even after operation, becomes uncertain.
Can a torn cuff be fixed by medicines or physiotherapy?
There are no medicines which can heal the torn tendons, not even physiotherapy can heal tendons. In cases with small tears, by strengthening the friendly neighbouring muscles, it's possible to compensate for functions of the torn muscle. Tendons are like rubber band, once torn, the torn ends are pulled apart by attached muscles. If one tendon is torn, the load goes to other tendons, and with time the tear extends into other tendons. With time, the gap between the torn ends increasing. The muscles attached to these tendons lose their bulk due to not being in use (disuse atrophy). In fact, with not in use for long time, the muscle fibres get replaced by fat, what is called fatty degeneration. This is a permanent loss of muscle.
What does surgical treatment entail?
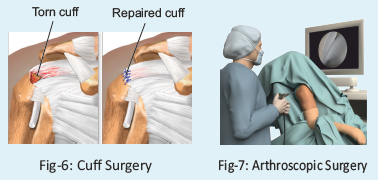
Surgery consists of attaching the torn tendons back to where they are supposed to be (Fig-6). This is the way torn cuff has been treated for ages, the only recent change is that now this all is done by key-hole (arthroscopic) surgery. In this technique, 3 or 4 small (1 cm) holes are made on the shoulder. Through one hole a camera is introduced, and inside the joint is seen on a TV monitor (Fig-7). Two or three further holes are made through which fine instruments are brought in. The benefit of key-hole surgery are: less pain, less cutting, quicker recovery and fewer complications. In vast majority it is possible to repair the cuff by this technique, but in some it's wiser to do mini open method to achieve a secure repair. This decision is often taken on the operation table.
How much does it cost?
Cost varies from case to case, depending upon the size of the tear. On an average, it costs from 1.5 L to 2.5 Lac* in a sharing category. We will be able to give you an estimate at the time of finalisation of the date.
How much time does the operation take?

Actual operation takes about 1.5 to 2.0 hours, but pre - operation (anaesthesia, positioning etc.) takes additional one hour. After surgery, you are kept in recovery area, and shifted to room once you are fully awake. The operation is done under general anaesthesia with nerve block (from your neck) for post-operative pain relief.
Is it a painful operation?
The operation is done under general anaesthesia, hence no pain at all, while operating. In the post op period we control the pain by blocking pain nerves at the neck or giving intra venous medicines. On a scale of 0-10, we try to keep the pain within less than 3 range, which is very much tolerable.
How successful is the operation?
It's overall a reasonably successful operation. The success depends upon the quality of repair, healing of tendon, and post-op physiotherapy. Broadly speaking, there are three partners to contribute to the success of the operation
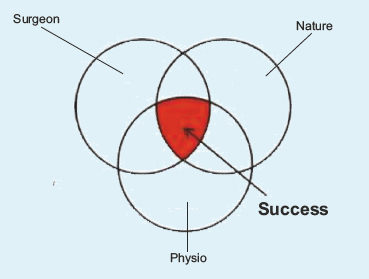
- The surgeon, who does the job of fixing the tendons back to its place. We have been doing this surgery for years and have acquired the necessary expertise. We record all operations and give the recorded CD to the patient.
- Mother nature, which has to make the tendon heel to its site of fixation - a process of natural healing of tissues. It varies from patient to patient, depends upon how old the tear is, age of the patient etc.
- Patient, who does physiotherapy to re-educate the torn muscles which often go into 'sleep mode'.
Any of the three not working well can lead to failure. Failure may mean partial success or no success. Fortunately, good 80 percent heal up well.
The following are the general factors that afect results of the treatment of torn rotator cuff.
- Age at which the tear happens – older the patient, poorer the healing capacity.
- Size of the tear - whether it is involving one, two or three tendons.
- Whether the tear was primarily traumatic or degenerative. Healing is worse in the latter.
- How retracted (pulled away) the tendon is from its original attachment.
- How long after injury is the surgery being done - more the delay, lesser the healing potential.
- What is the severity of muscle wasting over the period, from injury to operation?
- Is there, if any, permanent changes in the muscle (atrophy) as seen on MRI?
How much time does it take to recover?
It varies from case to case.* Small tears heal up fast and one can do most day-to-day activities within 1 to 2 months. Healing can be considered in three phases: (a) Phase 1: healing of tendon-6 weeks; (b) Phase 2: restoration of joint mobility and early re-education of the torn muscles-6 weeks; and (c) Gaining back the strength of the muscles (12 weeks to 24 weeks). One can perform day-to-day functions after 2 months. Post-op physiotherapy has a lot of role to play. We train patients to do exercises themselves with supervision by our trained physio. Some patients need more supervised physiotherapy. Sometimes an injection is given in shoulder to hasten the recovery process. Occasionally the shoulder gets stiff, and may have to be manipulated under anaesthesia.
What are the possible risks of surgery?
The surgery is generally safe. There are some standard risks which are associate with any surgery. Some of these are mentioned below for the sake of completion, and not to alarm.
Anaesthesia Risk: There are risks of putting anybody under anaesthesia. These range from as minor as nausea and vomiting due to some medication, to serious complications such as drug reaction, fall in BP, rarely heart attack due to stress etc. We do pre-op work up to make sure that we understand your body.
Surgical risk: The only serious risk is infection, which luckily occurs only 1 in 500 patients. We take all precautions to keep it within reasonable limits. The other risks are non-healing of the tendon, re-rupture of the tendon, stiff shoulder, persistent unexplained pain etc.
What are the highlights of our technique of rotator cuff repair?
- We use one-time use (disposable) tools to maintain lowest possible risk of infection.
- We use self-dissolving (bioabsorbable) anchors (a kind of fixation device).
- We use double-row fixation wherever required.
- We allow controlled movements of the shoulder, the very next day.
- We allow bath the very next day.
- We have devised a home- based physiotherapy programme with a few visits to our shoulder trained physios.
- The surgeon and physio work in close coordination.
- The surgeon is available 24x7, in case of any emergency.
Our philosophy: Most important, we have a philosophy of treatment. We take every patient as a human being with different requirements – physical and psychological. We customize our treatment to patient's need. Our aim is to give our patient the experience of having gone through the treatment, what we would expect for our own relative. For us, by choosing us their doctor, the patient is giving us a great honour, and we value it. To showcase that we care, all our operated patients have direct access to cellphones of our team, including that of the chief surgeon.
MAP